Transformation in Homecare
As many of you may be aware, Australia's Aged Care sector, and specifically the Homecare space, is undergoing significant transition with a number of reformed funding models and programs being legislated into effect over the coming years.
Support at Home Program
In addition to the reform relating to the 2023 Aged Care Act, from July 2023, the Support at Home Program will replace the following existing programmes and packages:
- Commonwealth Health Support Programme (CHSP)
- Home Care Packages (HCP)
- Short-Term Restorative Care (STRC) Programme
- Residential Respite programs
On March 8, 2022, our Clinical Excellence team participated in a webinar run by the Department of Health, which provided an update on the new Support at Home program's design, challenges, language and what to expect over the coming months. The webinar may be viewed here.
Support at Home FAQs
Why are the Support at Home reforms occurring?
- To better ensure Senior Australians get the support they need when and where they need it
- To make in-home Aged Care easier and simpler to use
- To increase value for money
- To improve accountability for quality and safety
What will the Support at Home Program improve?
The new program will focus on supporting individuals, tailored care, clarity, regulation and competition. It aims to do this through the following:
- Tailored care specific to the individual's needs rather than care to fit within a package level, model or formula
- Assistive Technologies, Goods and Modifications can be purchased for the individual's needs, when they need them, rather than only being available after a certain level of funds have been saved up
- Service providers will be paid quicker at the point of delivery and with streamlined reporting obligations
- Individuals will have greater choice between providers
An Integrated Assessment Tool
A new assessment tool is being developed to better match services to an individual's needs. The new tool will replace existing assessments such as: ACAT, RAS and NSAF and will be applicable for home care, residential aged care, transitional care and respite.
The way the assessment is conducted will depend upon the answers provided to each question, in a trigger-point model.
The assessment's outcomes will provide classes of funding for the individual's assessed care needs for a range of domains including:
- General and Personal Health
- Functional Decline
- Cognition
- Behaviour
- Medical Conditions
- Carer Support
Further information on the new Integrated Assessment Tool will be released through 2022, with its expected launch to be in July 2023.
Changes for Clinicians & Clients
Individualised Assessment Outcomes
Following their assessment using the new Integrated Assessment Tool, the individual will receive an Individualised Support Plan. The plan (outlined in an example below), will provide a guide on the service required and the frequency (or funding associated)- against each domain.
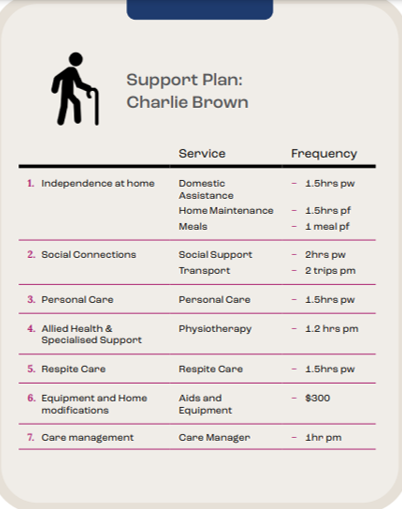
The Support Plan will be created by the assessor, with assistance and guidance from the individual. Much of this plan will consist of "frequency and level of support" rather than a "dollar value". However, some domains will continue to list requirements in monetary figures (further information below).
Home Modifications and Goods, Equipment and Assistive Technologies (GEAT)
The Department is still working on a plan to make access to Home Modifications and GEAT easier and cheaper to access for all. They have confirmed, that no longer will individuals need to "save" and/or "accumulate" enough funds to receive these important supports to maintain independence. The requirement for these supports will be within the new Integrated Assessment Tool, but consultation on this is ongoing.
Short Term Restorative Care (STRC)
Presently, the STRC package is available for up to eight weeks. Under the Support at Home Model (which STRC will be integrated into), services will now be available for up to twelve weeks with a greater focus on reablement and restoring one’s independence. Under the integrated model, should an individual require ongoing services at the end of their initial twelve-week period, they will undergo a reassessment which may recommend ongoing reablement or greater support services to match the individual's needs.
Unspent Funds
No longer will unspent funds be able to be accumulated and/or pooled. Similarly, providers will only be paid for the services delivered. If an individual were to go on a holiday and not require cleaning and/or in-person rehabilitation services, the individual will not accrue this money for "future use" and the provider will not be paid for a service not delivered.
Care Manager
The termed role "Case Manager" will be replaced by "Care Manager" under the Support at Home Program.
Regional and Remote Clients
Grants (yet to be formally announced) will be available for clinicians and providers to deliver services to clients residing in remote and/or difficult to service areas.
There are a number of workshops relating to the Support at Home Program and the upcoming reform to the Aged Care Act, to be announced throughout the remainder of 2022.
We expect these changes to fundamentally change how services are funded, managed and delivered in the Homecare space; with improved quality and accessibility to Vivir's Allied Health services and care being fundamental to these changes.
If you have any questions or would like additional information, please reach out to our team.








